The BC Nurses’ Union (BCNU) has partnered with Pacific Blue Cross to administer the new Nurses’ Bargaining Association (NBA) Supplemental Mental Health Benefit (SMHB). The purpose of this benefit is to address the need for enhanced mental health support for BCNU members covered by the Nurses’ Bargaining Association (NBA) provincial collective agreement. For more information about the application process visit https://www.bcnu.org/member-services/bursaries/smhb
If you don’t find answers to your questions about registering with Pacific Blue Cross (PBC) or accessing your account below, please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
General Inquiries
-
What does the NBA SMHB plan cover?
The NBA SMHB plan will cover mental health services rendered by registered psychologists, registered clinical counsellors, and registered social workers and iCBT (online Cognitive Behavioral Therapy).
-
Who is covered under the NBA SMHB plan?
The member is the only person eligible for the plan. Your spouse, or any other dependent (child, post-secondary student) is not eligible to receive this benefit.
-
Where can I find my member ID card for the NBA SMHB plan?
Please log into your existing Member Profile account, or register for Member Profile to view, email and/or print your digital member ID card.
-
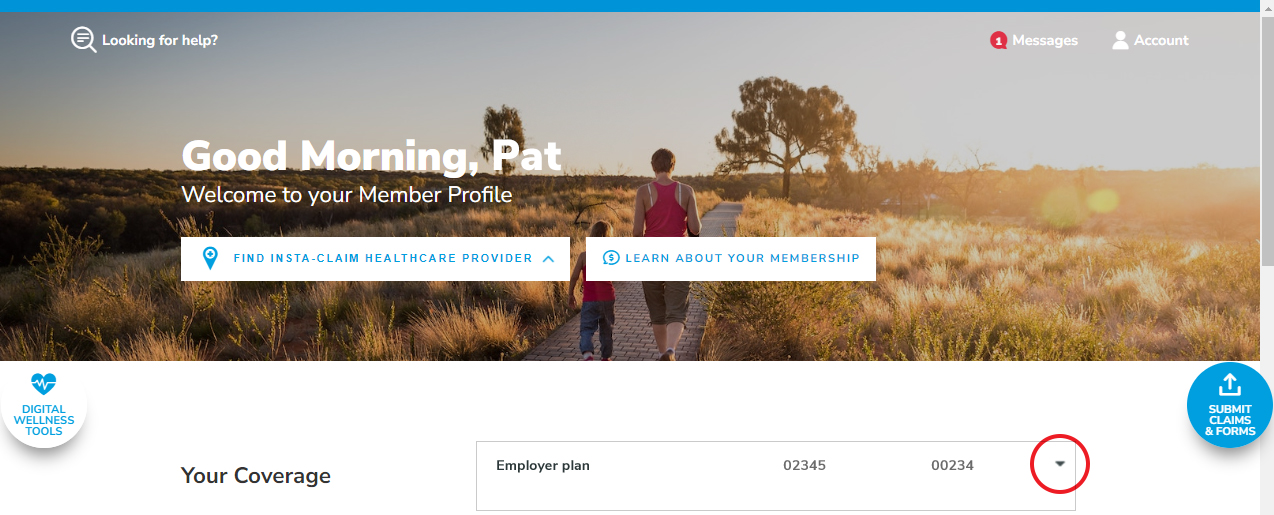
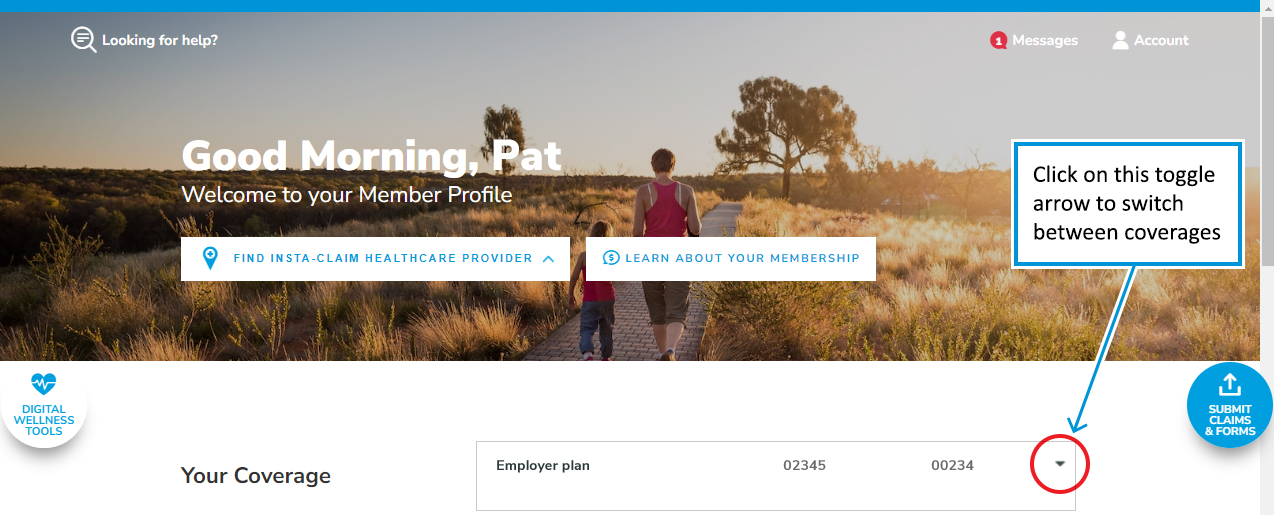
Once you have signed into your Member Profile account. If you see a toggle arrow to the right of Your Coverage (as shown below), this will let you toggle to view your other coverages that are linked, including the NBA SMHB plan.
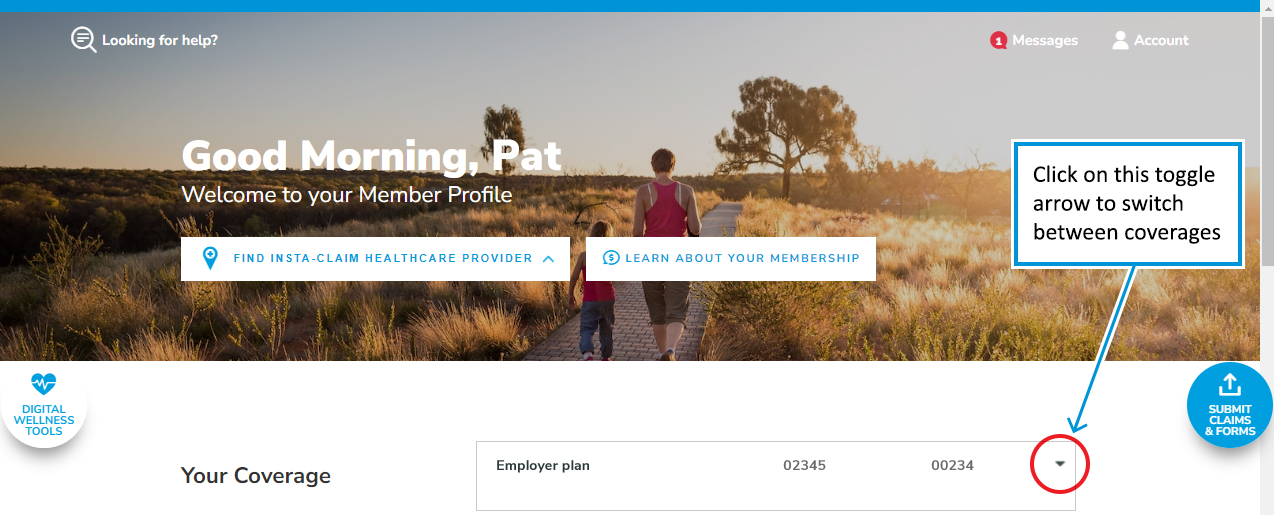
-
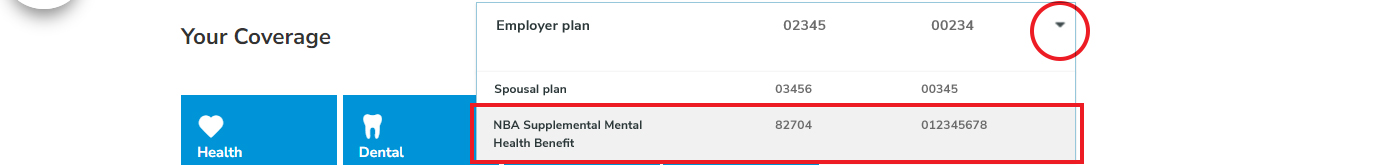
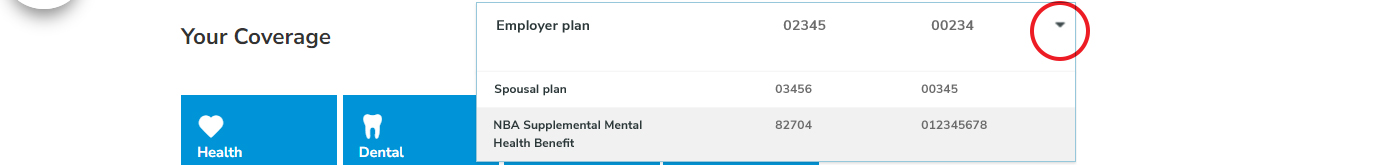
Click the toggle arrow. To view your NBA SMHB plan, select it from the list. This will take you to the main page of your Member Profile for the NBA SMHB plan.
-
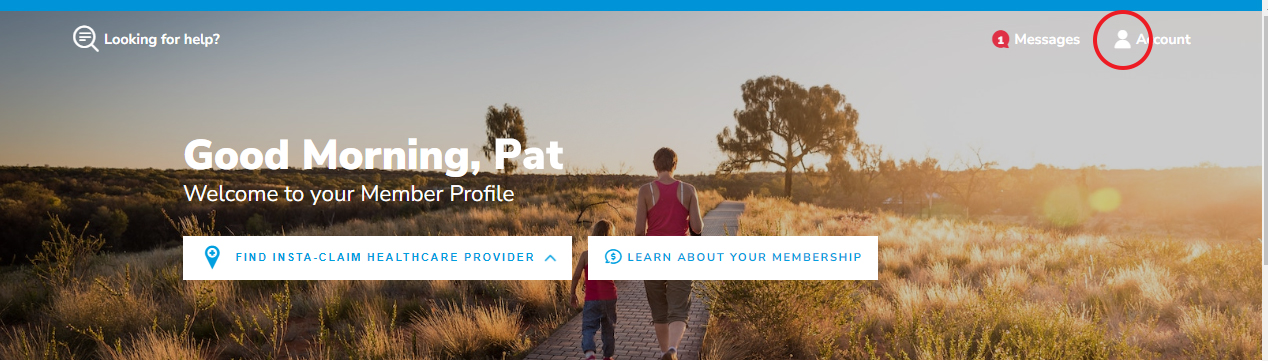
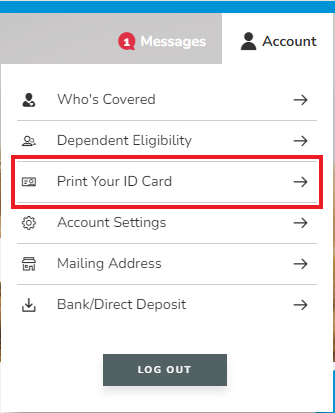
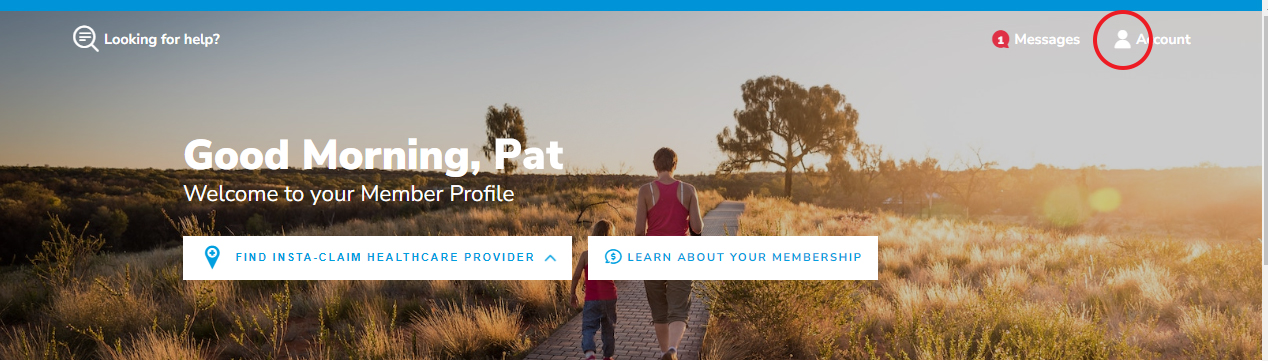
To view and email/print your NBA SMHB plan ID card, click on Account in the top right corner of your screen.
-
Select Print Your ID Card.
If you do not see the toggle arrow or, if you do not see all your PBC coverages listed, this means that your records have not been linked. This could happen if the information submitted to the NBA SMHB plan differs from what was submitted for your existing Extended Health plan. Please contact us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583) so we can link your records, allowing you to see the toggle arrow on Member Profile.
Once you can see the toggle arrow on Member Profile and/or you’re able to see and select your NBA SMHB plan, you can follow the instructions above to view, print or email your NBA SMHB plan ID card.
Please note, our Call Centre agents will not be able to link your records over the phone, but they will submit the request for you. This is a manual process that may take up to 6 weeks to complete.
If you have incurred expenses, to avoid processing delays please hold onto your receipts to submit online once your coverages are linked or, you can also submit your claim by completing and mailing the Standard Health Claim form.
For more information, please visit our ID card FAQs.
-
-
How does the NBA SMHB plan work?
The NBA SMHB plan is used to supplement what your employer-sponsored Extended Health plan covers for mental health services. All claims will need to be submitted first through your employer-sponsored extended health plan(s) and/or your partner’s plan (if applicable); the outstanding amount not paid can then be processed under the NBA SMHB plan.
Please be aware that once your employer and/or partner’s Extended Health plan maximums for this benefit have been reached and your PBC plans are linked, mental health expenses will be automatically processed under the NBA SMHB plan.
If your plans are not linked, please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
-
What date did the NBA SMHB plan become effective?
The NBA SMHB plan was activated in the Pacific Blue Cross (PBC) system on June 3, 2024. Once enrolled on the PBC system, members can immediately submit mental health claims with a date of service as early as March 31, 2023.
-
What is the claiming deadline for the NBA SMHB plan?
The claiming deadline for claims with dates of service between March 31, 2023 – December 31, 2023, is December 31, 2024.
The claiming deadline for claims with dates of service for January 1, 2024 and thereafter have a submission deadline of June 30 of the following year.
Example: If the expense was incurred on February 18, 2024, it would need to be submitted to PBC under the NBA SMHB plan by June 30, 2025, to be considered as an eligible expense under the NBA SMHB plan.
-
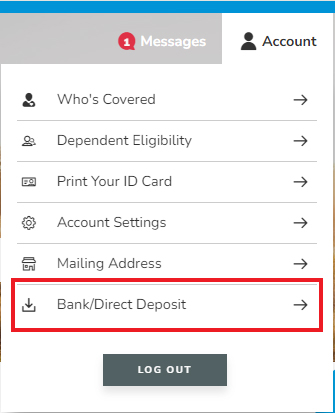
Where do I set up direct deposit under the NBA SMHB plan?
To be paid electronically from your NBA SMHB plan, you will need to set up Direct Deposit under the NBA SMHB plan so that reimbursements are paid quickly and directly to your bank account. If you don’t add your direct deposit information, reimbursements will be mailed as a cheque to your address on file.
To setup your direct deposit, once signed into your Member Profile account, if you see the toggle arrow next to Your Coverage on the main page of your Member Profile account (as shown below), this means that your records have been linked. Click on the toggle arrow and you will see a list of your linked coverages. To view your NBA SMHB plan, select it from the list. This will take you to the main page of your Member Profile for the NBA SMHB plan. Click on Account in the top right corner of your screen.
-
Select Bank/Direct Deposit.
-
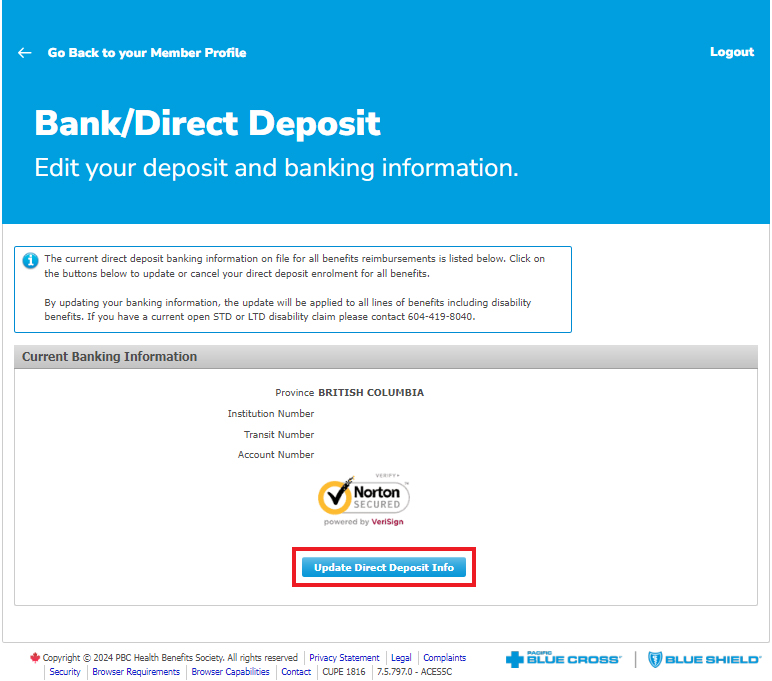
Next click on Update Direct Deposit Info.
-
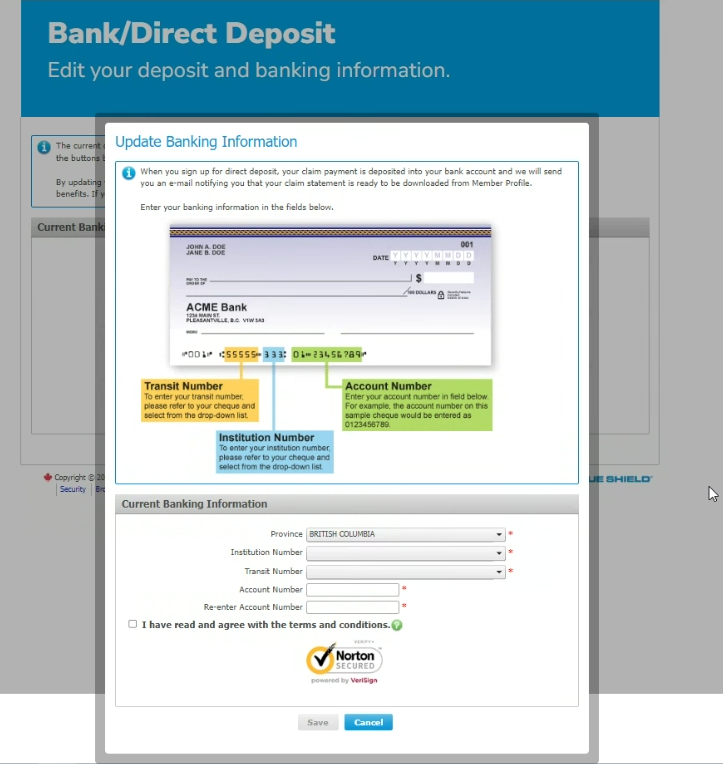
Now enter your banking information, read, and agree to the Terms and Conditions, and then click Save. Before you click Save, please ensure that the banking information you have entered is correct.
-
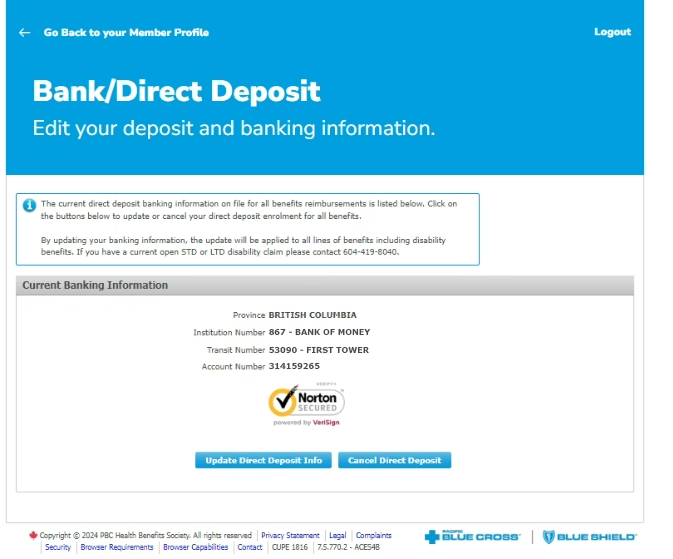
Congratulations, your direct deposit has been set up and you will receive electronic payments for eligible claims under the NBA SMHB plan. Now you will see your banking information on the screen. Please re-review this information for accuracy.
-
Benefits Information
-
What does the NBA SMHB plan cover?
The NBA SMHB plan will cover mental health services rendered by registered psychologists, registered clinical counsellors, registered social workers, and iCBT (online Cognitive Behavioral Therapy).
-
Do Reasonable & Customary charges apply to the NBA SMHB plan?
The NBA SMHB plan up to 20 percent more than the PBC Reasonable and Customary fees for mental health providers. These higher fees are the allowable per visit limits for the NBA SMHB plan. However, it is important to note that if your provider charges more than this allowable amount, you will be responsible for paying the difference.
-
Is there a maximum amount provided under the NBA SMHB plan?
There is a lifetime limit of $5,000 per person.
-
What does my Extended Health plan with PBC cover for mental health services?
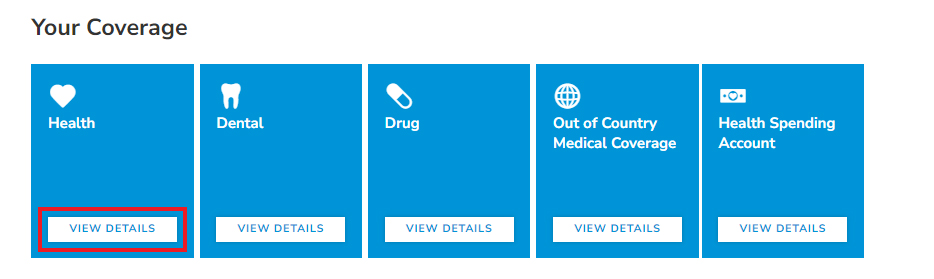
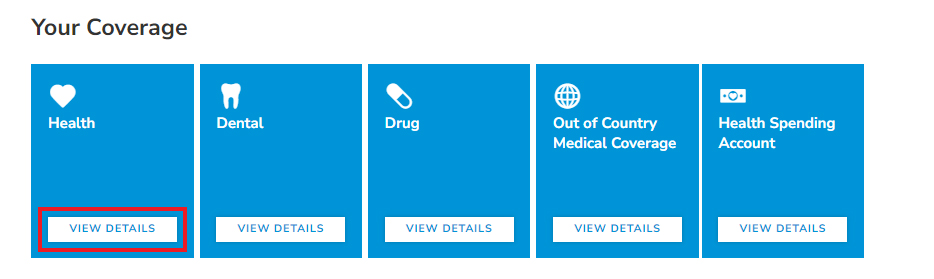
Please check your coverage by logging into your Member Profile account and click on View Details under the Health tile to view your coverage under all of your plans (e.g., your employer and/or your partner’s plan [if applicable]).
-
I have signed into MY Member Profile account under my Extended Health plan, where can I see the details of my NBA SMHB plan?
Once signed into your Member Profile account, if you see the toggle arrow next to Your Coverage on the main page of your Member Profile account, this means that your records have been linked. Click on the toggle arrow and you will see a list of your linked coverages. To view your NBA SMHB plan, select it from the list. This will take you to the main page of your Member Profile for the NBA SMHB plan. Click on View Details under the Health tile to view your NBA SMHB coverage.
If you do not see the toggle arrow or, if you do not see all your PBC coverages listed, this means that your records have not been linked. This could happen if the information submitted to the NBA SMHB plan is different than what was submitted for your employer’s Extended Health plan. Please contact us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583) so we can link your records, allowing you to see the toggle arrow on Member Profile.
Please note, our Call Centre agents will not be able to link your records over the phone, but they will submit the request for you. This is a manual process that may take up to 6 weeks to complete. If you have incurred expenses, please hold on to your receipts. Once you see the toggle arrow on Member Profile and you’re able to see and select your NBA SMHB plan, you can follow the instructions above to view the details of your NBA SMHB plan.
Information about Linked Coverages
-
How can I confirm that my PBC plans will automatically coordinate when I submit a claim?
If all your coverages are with PBC
For the automatic coordination of payment, your enrolment records under all your PBC coverages must be linked, e.g., your employer plan, your partner's PBC plan (if applicable) and/or the NBA SMHB plan. If all your PBC coverages are linked, the system will recognize this and automatically process the claim under all PBC coverages in the correct order, regardless of which plan the claim is submitted under.
To check if your enrolment records are linked, sign into your Member Profile account. If you see a toggle arrow to the right of Your Coverage this will let you toggle to view your other PBC coverages that are linked, and should include the NBA SMHB plan.
When you click the toggle arrow you will be able to see all your linked coverages. If you see all your PBC coverages, your claims will automatically coordinate under the PBC coverages.
If you do not see the toggle arrow or, if you do not see all your PBC coverages listed, please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays. Once you see the toggle arrow on Member Profile and/or you’re able to see all of your PBC coverages, your claims will automatically coordinate under the PBC coverages.
If you also have coverage under your partner’s plan that is not with PBC
Please contact PBC in advance of submitting a claim if you have coverage under your partner’s Extended Health plan with another insurance provider. Please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
When you contact us, we will update your record to ensure claims do not automatically process under the SHMB plan before your coverage under your partner’s Extended Health plan with the other insurance provider.
After we have updated our files to note your other coverage the process for submitting your claims is as follows:
- You or your provider* will need to submit to your employer’s plan with PBC first. Once processed and you know how much your employer’s plan with PBC paid towards the expense, if there is an outstanding unpaid balance you or your provider can then submit the claim to your partner’s plan with the other insurance provider. You will need to disclose to your other insurance plan how much was paid by your employer’s plan. Once processed by the other insurance provider and you know how much the other insurance provider paid towards the expense, if there is an outstanding unpaid balance you or your provider* can then submit the claim online to your NBA SMHB plan with PBC.
- When you or your provider* submit this claim to your NBA SMHB plan with PBC, you must submit for the total amount of the expense, indicate “Yes” to the COB question, and enter the combined amount paid amount by your PBC plan and/or other insurance provider. This will ensure your claim is coordinated to only pay the balance and will help your lifetime maximum under the NBA SMHB plan last longer.
Please be advised, you will need to include an Explanation of Benefits statement (this is an insurance provider’s written explanation regarding a claim, showing what they paid) from the other carrier.
-
If you had already submitted a claim to PBC and it paid under the NBA SMHB plan before notifying PBC of your partner’s coverage with another insurance provider, we will also adjust your claim to reverse the payment under your NBA SMHB plan. You or your provider can then submit the claim to your partner’s plan with the other insurance provider. You will need to disclose to the other insurance provider how much was paid by your employer’s plan PBC plan. Once processed by the other insurance provider and you know how much the other insurance provider paid towards the expense, if there is still an outstanding unpaid balance, you or your provider* can then submit the claim online to your NBA SMHB plan with PBC.
When you or your provider* submit this claim to your NBA SMHB plan with PBC, you must submit for the total amount of the expense, indicate “Yes” to the COB question, and enter the combined amount paid amount by your PBC plan and/or other insurance provider. This will ensure your claim is coordinated to only pay the balance and will help your lifetime maximum under the NBA SMHB plan last longer.
Please be advised, you will need to include an Explanation of Benefits statement (this is an insurance provider’s written explanation regarding a claim, showing what they paid) from the other carrier.
* Please note, currently registered psychologists are the only mental health providers that can submit claims on your behalf through PROVIDERnet (PBC’s provider portal for claim submission and inquiries).
-
Is there anything I need to do if my PBC coverages are linked?
If you see all of your PBC coverages when you sign into your Member Profile account, all you need to do is set up your direct deposit information under your NBA SMHB plan so that reimbursements are paid quickly and directly to your bank account. Setting up direct deposit under the NBA SMHB plan will avoid payment delays as reimbursements will be mailed as a cheque to your address on file.
If you do not see all your PBC coverages, please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays. Once you see you’re able to see all your PBC coverages, you can setup your direct deposit information under the NBA SMHB plan.
-
Why is it important for my enrolment records to be linked/merged?
Linking your records will allow you to have a single Member Profile account and allow the system to automatically coordinate claim payments between all your PBC plans, including any coverage under a partner’s plan with PBC (if applicable).
For example, if your enrolment records are linked and you submitted a claim for a psychology visit, the system will automatically recognize your coverage under your employer’s Extended Health plan, your partner’s plan with PBC (if applicable), and the NBA SMHB plan, processing the claim under each policy without requiring you to submit three separate claims.
If you also have coverage under your partner’s plan that is not with PBC, please contact us in advance of submitting claims to ensure claims do not automatically process under the SHMB plan before your coverage under your partner’s Extended Health plan with the other insurance provider.
Please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
Coordination of Benefits Information
-
If I am covered on more than one plan, what order do I submit claims in?
If you are covered under more than one plan, you are required to submit your claims to your own Extended Health plan first. Any remaining balance may be claimed through your spouse's plan (if applicable). If a balance remains, this can be submitted to your NBA SMHB plan last.
-
What if I have coverage under my partner’s plan with PBC?
If you have coverage under your partner’s plan with PBC, your mental health claims should first be submitted to your employer’s Extended Health plan, then your partner’s plan, and then to the NBA SMHB plan. If your plans are linked, mental health expenses will be processed automatically under all coverages that are linked when you submit your claim under your employer-sponsored extended health plan. By following these coordination rules, your lifetime maximum under the NBA SMHB plan will last longer.
-
What if I also have coverage under my partner’s plan that is not with PBC?
Please contact PBC in advance if you have coverage under your partner’s Extended Health plan with another insurance provider. Please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
When you contact us, we will update your record to ensure claims do not automatically process under the SHMB plan before your coverage under your partner’s Extended Health plan with the other insurance provider. After we have updated our files to note your other coverage the process for submitting your claims is as follows:
You or your provider* will need to submit to your employer’s plan with PBC first. Once processed and you know how much your employer’s plan with PBC paid towards the expense, if there is an outstanding unpaid balance you or your provider can then submit the claim to your partner’s plan with the other insurance provider. You will need to disclose to your other insurance plan how much was paid by your employer’s plan. Once processed by the other insurance provider and you know how much the other insurance provider paid towards the expense, if there is an outstanding unpaid balance you or your provider* can then submit the claim online to your NBA SMHB plan with PBC.
When you or your provider* submit this claim to your NBA SMHB plan with PBC, you must submit for the total amount of the expense, indicate “Yes” to the COB question, and enter the combined amount paid amount by your PBC plan and/or other insurance provider. This will ensure your claim is coordinated to only pay the balance and will help your lifetime maximum under the NBA SMHB plan last longer.
Please be advised, you will need to include an Explanation of Benefits statement (this is an insurance provider’s written explanation regarding a claim, showing what they paid) from the other carrier.
* Please note, currently registered psychologists are the only mental health providers that can submit claims on your behalf through PROVIDERnet (PBC’s provider portal for claim submission and inquiries).
-
What if I don’t have coverage under PBC for my Extended Health plan?
If you have coverage for Extended Health with another insurance provider and it covers mental health services, you or your provider will need to submit to your other plan first. Once processed and you know how much the other insurance provider paid towards the expense, if there is an outstanding unpaid balance you or your provider* can then submit the claim online to your NBA SMHB plan with PBC.
When you or your provider* submit this claim to your NBA SMHB plan with PBC, you must submit for the total amount of the expense, indicate “Yes” to the COB question, and enter the amount the other plan paid. This will ensure your claim is coordinated to only pay the balance and will help your lifetime maximum under the NBA SMHB plan last longer.
Please be advised, you will need to include an Explanation of Benefits statement (this is an insurance provider’s written explanation regarding a claim, showing what they paid) from the other carrier.
* Please note, currently registered psychologists are the only mental health providers that can submit claims on your behalf through PROVIDERnet (PBC’s provider portal for claim submission and inquiries).
-
What if I do not have an extended health plan?
If you have no other Extended Health coverage (either with another insurance provider or PBC) for mental health services, you or your provider* will need to submit directly to the NBA SMHB plan.
* Please note, currently registered psychologists are the only mental health providers that can submit claims on your behalf through PROVIDERnet (PBC’s provider portal for claim submission and inquiries).
-
What if my claim did not process under all of my PBC plans?
If your claim was not processed under all of your PBC coverages, please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
-
What if my partner’s external coverage (not with PBC) was missed when my claim was processed?
If your external coverage under your partner’s plan was missed during your claim, please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
When you contact us, we will update your record to ensure claims do not automatically process under the SHMB plan before your coverage under your partner’s Extended Health plan with the other insurance provider.
-
What if my mental health provider submitted a claim for me and it paid under my employer’s plan and NBA SMHB plan, but I want to submit part of the claim to my partner’s external coverage (not with PBC)?
If your external coverage under your partner’s plan was missed during your claim, either you or your provider can call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
When you contact us, we will update your record to ensure claims do not automatically process under the SHMB plan before your coverage under your partner’s Extended Health plan with the other insurance provider.
-
What amounts should be entered when submitting an online claim, when a portion of the expense has been paid by your and/or your partner’s Extended Health Care plan with PBC or another Insurance provider?
Claims should not be submitted to this plan until the claim has been fully adjudicated under your existing Extended Health plan and/or partner plan. Once you have received the final decision from your existing Extended Health Care plan and/or partner’s Extended Health Care plan, if they have not been fully reimbursed, the outstanding amount can be submitted to the NBA SMHB plan by ensuring the following fields are entered as follows:
Field Name What to enter Example Total amount of the expense
Enter the full amount of the service/expense, before any insurance has reimbursed.
Service Bill $150.00 Total amount of expense $150.00 In this example, PBC member EHC plan paid $80.00 Partner's EHC plan $20.00 Amount paid by Pacific Blue Cross/other insurance plan $100.00 Has this expense been submitted to another insurance plan?
Yes.
Amount paid by Pacific Blue Cross/other insurance plan
Enter the amount paid by all insurance plans, including all Extended Health Care plans, including PBC, combined.
This will ensure your claim is coordinated to only pay the remaining balance and will help your lifetime maximum last longer under the NBA SMHB plan.
Claims Processing Information
-
How do I submit my mental health claim online?
If you are seeing a psychologist, you can ask if they will bill PBC directly on your behalf. Otherwise, if not, and your Extended Health coverage is through PBC, you can log into your Member Profile using your employer’s Extended Health policy number.
You will be able to submit your claim by clicking the Submit a Claim button and you will be walked through the process.
If your coverages are linked, the claim will be processed under all of your PBC coverages in the correct order.
If your claim was not processed under all of your PBC coverages, they may not be linked. Please call us at 604-419-2000 or toll free at 1-877-PAC-BLUE (1-877-722-2583), Monday to Friday, 8 am to 4:30 pm, excluding statutory holidays.
-
How long does it take for my claims to be paid?
If your claim is below the allowable limit per visit and is submitted electronically, it should be processed the same day and payment should be in your account within three business days.
If your claim is over the allowable limit per visit, it will undergo review by a Claims Examiner. Please note, this is a manual process and can take between 4 – 6 weeks to complete.
-
Can my mental health provider submit a claim on my behalf?
Yes. Please note, currently registered psychologists are the only mental health providers that can submit claims on your behalf through PROVIDERnet (PBC’s provider portal for claim submission and inquiries).
-
What if I go to a mental health provider that is not registered for PROVIDERnet?
If you go to a mental health provider not registered for PROVIDERnet (PBC’s provider portal for claim submission and inquiries), you will need to pay for the mental health services and then submit the claim. For convenience and faster payment submit online claims through Member Profile, or the mobile app. You can also submit your claim by completing and mailing the Standard Health Claim form.
-
Can I or my mental health provider submit claims directly to PBC under the NBA SMHB plan without submitting to my employer-sponsored and/or partner’s plan?
No. If your coverages are linked, the system will recognize this and automatically process the claim under all PBC coverages in the correct order, regardless of which plan the claim is submitted under.
Claims for expenses before the NBA SMHB plan was set up
-
What if I had an outstanding amount for mental health services that were not covered by my employer’s Extended Health plan before the NBA SMHB plan was set up in June 2024?
After you are enrolled in the NBA SMHB plan, you can submit mental health claims with dates of service from March 31, 2023, onward under the NBA SMHB plan if they have not been fully reimbursed through your employer’s Extended Health plan and partner’s plan (if applicable). To do so, you will need to provide , you must submit the total amount of the expense, indicate “Yes” to the COB question, and enter the combined paid amount by your PBC plan and/or other insurance provider. This will ensure your claim is coordinated to only pay the balance and will help your lifetime maximum under the NBA SMHB plan last longer.
Please note, you will need to include an Explanation of Benefits statement (this is an insurance provider’s written explanation regarding a claim, showing what they paid) from the other carrier.
Claims with dates of service before March 31, 2023, are not eligible.
-
How do I submit my 2023 mental health expenses to PBC?
For claims with dates of service between March 31, 2023, and December 31, 2023, where you have already received reimbursement from your existing Extended Health plan and/or partner’s Extended Health plan, if they have not been fully reimbursed the outstanding amount can be submitted to the NBA SMHB plan by:
- Submitting the claim online through Member Profile or the PBC mobile app to get your reimbursement quickly and directly to your bank account. You will need to provide a copy of the receipt, as well as submitting the total amount of the expense, indicating “Yes” to the COB question and entering the combined paid amount by your PBC plan and/or other insurance provider. This will ensure your claim is coordinated to only pay the balance and will help your lifetime maximum under the NBA SMHB plan last longer.
Please note, you will need to include Explanation of Benefits statement(s) (this is an insurance provider’s written explanation regarding a claim, showing what they paid). Or, - Completing a paper claim form and ensuring you have attached all your receipts and any Explanation of Benefits statement(s), then mailing or dropping off the required documentation to PBC.
Mental health claims with dates of service from March 31, 2023, through to December 31, 2023, that have outstanding amounts not paid by the Extended Health plan must be received in our office under the NBA SMHB plan no later than December 31, 2024, to qualify for reimbursement.
- Submitting the claim online through Member Profile or the PBC mobile app to get your reimbursement quickly and directly to your bank account. You will need to provide a copy of the receipt, as well as submitting the total amount of the expense, indicating “Yes” to the COB question and entering the combined paid amount by your PBC plan and/or other insurance provider. This will ensure your claim is coordinated to only pay the balance and will help your lifetime maximum under the NBA SMHB plan last longer.
-
Is there a date that claims incurred in 2023 must be submitted to PBC to qualify for reimbursement?
Mental health claims with dates of service from March 31, 2023, through to December 31, 2023, that have outstanding amounts not paid by the Extended Health plan must be received in our office under the NBA SMHB plan no later than December 31, 2024, to qualify for reimbursement.