-
What is changing?
We now offer electronic pre-determination and claims processing for hearing products and services for MSDPR clients.
-
Why are you making these changes?
Through automation we can provide better service, help to streamline your administration of MSDPR clients, reduce your claims handling costs, and turn pre-determination confirmations and benefits claims around faster.
-
I’m a hearing provider. How will these changes affect me?
If you are registered for PROVIDERnet and direct deposit with Pacific Blue Cross, you now have the ability to process most product or service pre-determinations, as well as submit most benefits claims electronically on behalf of MSDPR clients. Plus, the direct deposit set-up ensures reimbursements from all Pacific Blue Cross plans are paid right into the bank account you set up on PROVIDERnet.
-
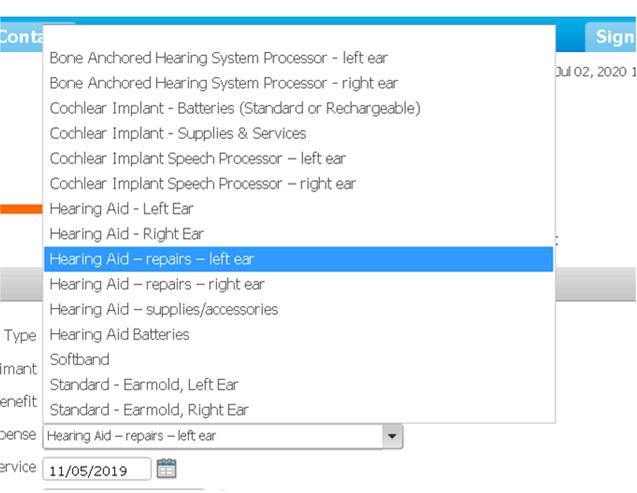
Are all service codes eligible for electronic processing?
There are a few service codes that are not currently available for electronic processing and will require manual submissions. These include service codes for Bone Anchored hearing system processors and parts, as well as Cochlear Implant speech processors and parts.
-
When did these changes take place?
Changes were rolled out on August 4, 2020.
-
Can I still send claims in manually?
Yes.
-
Will there be any changes to benefits coverage for MSDPR clients?
No. Benefit coverage amounts are not changing for hearing products or services for MSDPR clients.
Note: While coverage amounts are not changing, there will be a few new service codes to facilitate electronic billing.
-
How do I prepare for this transition?
Register as a provider with Pacific Blue Cross and sign up for PROVIDERnet and direct deposit (which is managed through PROVIDERnet). You will need to access PROVIDERnet in order to process claims and pre-determinations electronically and direct deposit to receive payments.
-
How do I sign up for PROVIDERnet?
To sign up for PROVIDERnet, go to the Hearing Provider Account Management page and follow the prompts.
Detailed instructions on how to sign up for PROVIDERnet are available in the Hearing Provider Reference Guide found on pac.bluecross.ca/provider.
-
How do I sign up for direct deposit or make changes to my existing information?
You must be registered for PROVIDERnet to set up or manage direct deposit. Detailed instructions on how set up or make changes to your direct deposit information are available in the Hearing Provider Reference Guide at pac.bluecross.ca/provider.
-
Will I get paid as soon as the claim is adjudicated if I submit through PROVIDERnet?
Payment dates will remain the same. However, instead of mailing a cheque we’ll deposit the reimbursement directly into the bank account you set up on PROVIDERnet.
-
How can I confirm MSDPR client eligibility for hearing services?
Confirming client identification. MSDPR clients will have either a British Columbia Driver’s Licence or British Columbia Services Card as their identification. This card will contain their Personal Health Number (PHN), which is unique to each individual. The policy number for MSDPR clients is 13139. To be eligible for coverage, MSDPR clients must reside in British Columbia.
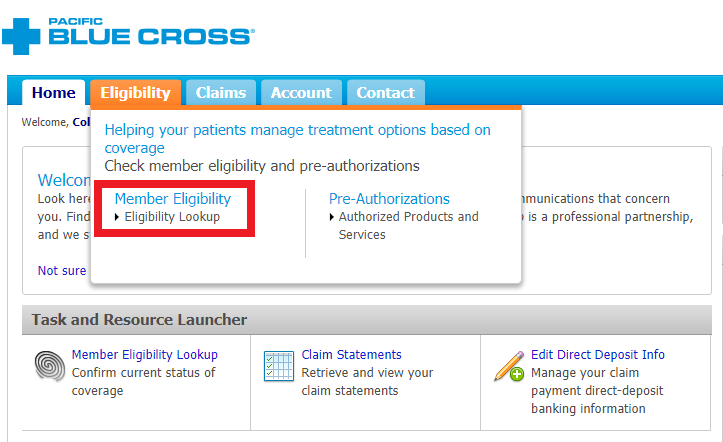
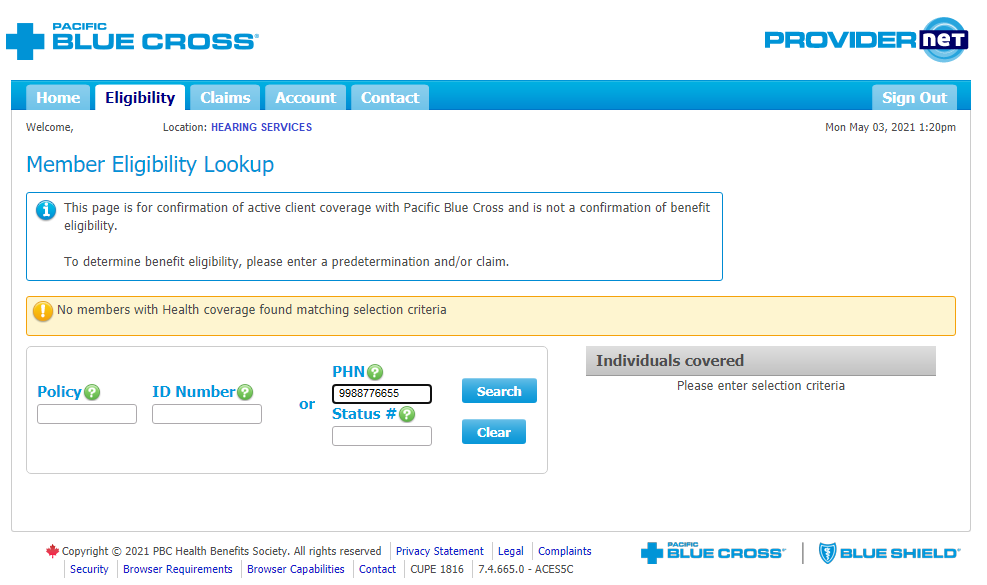
Confirming client’s available coverage. You are now able to check a client’s eligibility in PROVIDERnet. Simply go to the Eligibility tab menu option and select Member Eligibility > Eligibility Lookup
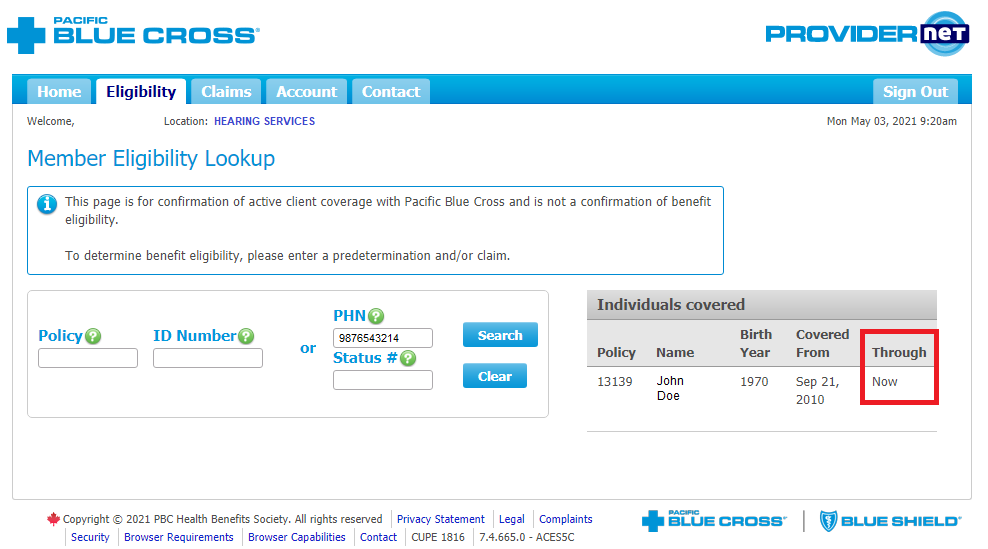
Enter the client’s Personal Health Number (PHN).
If a person shows as covered through “Now” on PROVIDERnet, that means they have active coverage for the current month.
This page is for confirmation of active client coverage with Pacific Blue Cross and is not a confirmation of benefit eligibility.
To determine benefit eligibility, please enter a pre-determination and/or claim.
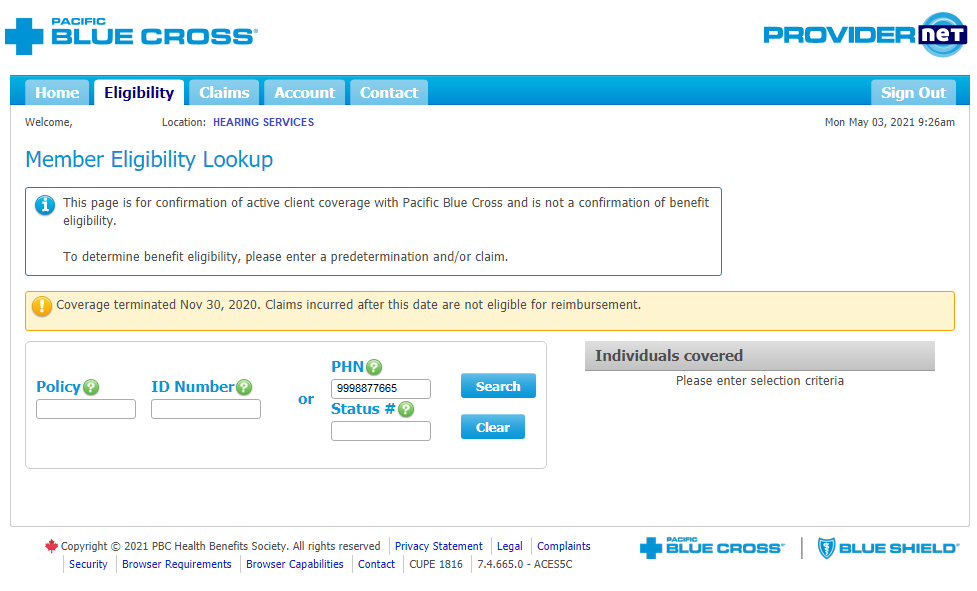
When a person does not have active coverage with Pacific Blue Cross, the system will provide you with a yellow alert message. There are two types of messages you could expect to see.
If a client no longer has coverage through the Ministry, the yellow box will indicate when their coverage ended.
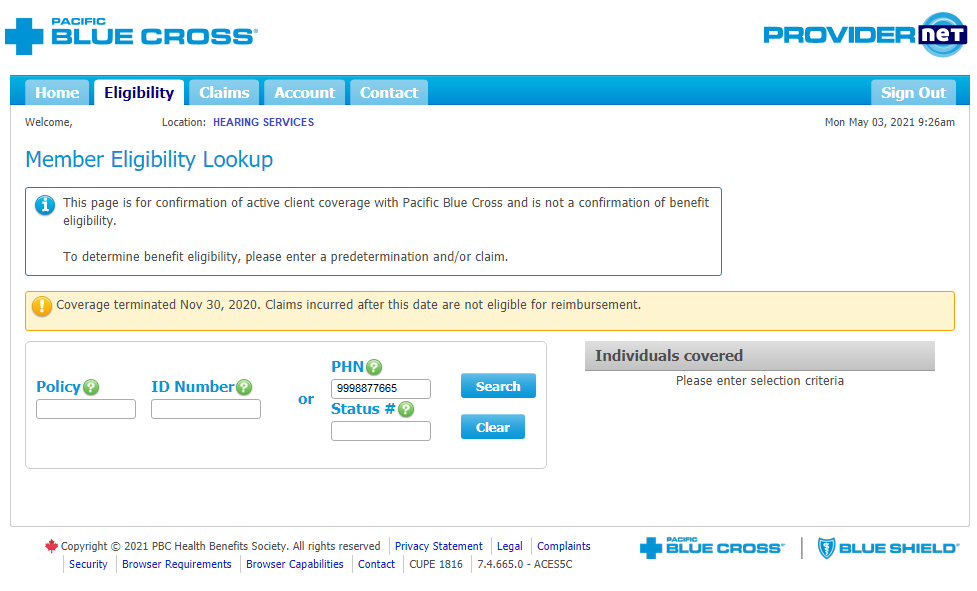
If the client is not found, the yellow box will indicate that “no members with health coverage found matching selection criteria.”
If the client is not found, the yellow box will indicate that “no members with health coverage found matching selection criteria.”
Alternatively, you can call the Pacific Blue Cross Ministry Department at 604-419-2780 or toll-free at 1-800-665-1297 to check eligibility.
Please note: Coverage under the Ministry plan is determined on a month-to-month basis. Thus, you must always confirm the client is active for the current month when determining benefit eligibility. If you submitted a pre-determination in one month but will be submitting the claim for services provided in the following month, please check eligibility prior to providing services or submitting the claim.
-
Which hearing services are covered for MSDPR clients?
Pacific Blue Cross will continue to follow existing plan provisions for eligible items such as standard hearing aids, repairs, batteries, supplies, and replacements.
- Hearing instruments are paid up to $2,000.00 per ear.
- New Hearing instrument purchases must include:
- Free assessment and 60-day trial of hearing instruments;
- 1-year supply of batteries (included in the purchase cost); and
- 1-time replacement coverage (paid at $300 per aid at the time of occurrence).
- Hearing instruments are eligible for replacement after three years from the purchase date.
Please Note — Pre-determinations are required for all hearing instrument claim reimbursements.
The plan may also consider coverage for bone anchored hearing aids and cochlear implant speech processors and supplies, but only when a standard hearing aid is not appropriate to meet the patient’s need. Additional supporting documentation may be required when requesting these types of hearing instruments.
For more information, please see the Hearing Provider Reference Guide at pac.bluecross.ca/provider
-
Are pre-determinations required before an MSDPR client’s claim can be processed?
Yes. All claims for hearing instruments submitted on behalf of MSDPR clients must have an approved pre-determination on file in order to be processed for reimbursement.
-
How do I submit a pre-determination for an MSDPR client electronically?
Detailed instructions on how to process a pre-determination electronically through PROVIDERnet for an MSDPR client are available in the Hearing Provider Reference Guide on pac.bluecross.ca/provider.
-
How do I submit a claim for an MSDPR client electronically?
Detailed instructions on how to process a claim electronically through PROVIDERnet for MSDPR clients are available in the Hearing Provider Reference Guide on pac.bluecross.ca/provider.
-
Can I submit a pre-determination under one provider ID and submit the claim under a different provider ID?
No. Both the pre-determination and the claim must have the same provider ID for the claim to be processed. If you need help directing your payment to a head office, please reach out to our Provider Relations Team at provider@pac.bluecross.ca.
-
If a patient has both MSDPR and First Nations Health Authority (FNHA) coverage, should I submit just one claim to Pacific Blue Cross?
If a patient has both MSDPR and FNHA coverage, you will need to submit two claims. Please submit the MSDPR claim first. Once that claim has been adjudicated and you have received a response message, you will be able to submit the claim under the patient’s FNHA plan.
-
I already have a PROVIDERnet account, will I need to create a new one to submit claims on behalf of MSDPR clients?
No. If you have an existing PROVIDERnet account, you do not need to take any further action. As of August 4, 2020, you will be able to submit claims on behalf of MSDPR clients, as well as FNHA clients.
-
How do I enter a claim for supplies/accessories for hearing aids, cochlear implants, and Bone Anchored hearing system parts?
When entering a claim for supplies/accessories for hearing aids, cochlear implants, and Bone Anchored hearing system parts, please put the description of the supply/accessory in the “Nature of Illness/injury” field.
For example, if you are submitting earhooks for a hearing aid, please select “Hearing Aid supplies/accessories”, and in the “Nature of Illness/Injury field”, please enter “earhooks”.

-
What happens if an MSDPR client’s hearing aid is lost, stolen, or broken?
In order for a client under the MSDPR Policy to receive a replacement hearing instrument, the original hearing instrument must have included the one-time replacement coverage. The fee for replacement coverage can be submitted to Pacific Blue Cross for consideration.
If you are submitting the claim electronically, please submit under “Hearing Aid – repairs”.
In the “Nature of Illness/injury” field, please indicate that this is a one-time replacement coverage charge.
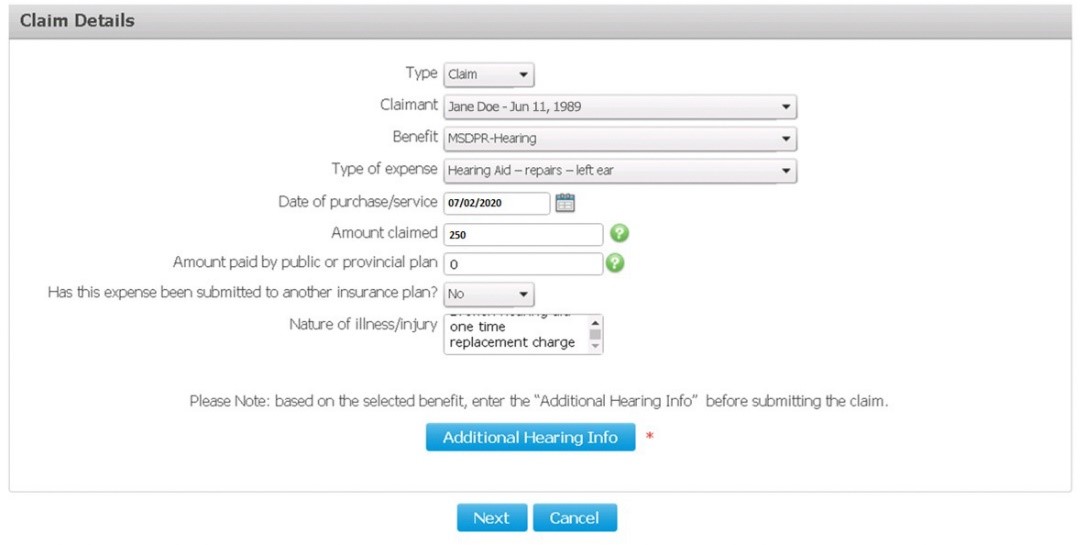
Finally, in the “Additional Information” screen, select “No” under the warranty section, then select “One Time Replacement.”
-
Where can I find the pre-determination/claim form?
You can find the pre-determination/claim form at https://www.pac.bluecross.ca/pdf-bin/ministry/0606.002.MinistryHearingInstrumentForm.pdf.
Please note that effective June 1st, 2021 manual submissions for Hearing will require the new updated pre-determination/claim form. Claims received on old forms will no longer be accepted after June 1st, 2021.
FAQ: Ministry of Social Development and Poverty Reduction – Digital management of hearing pre-determinations and claims.
As the benefits administrator for the Ministry of Social Development and Poverty Reduction (MSPDR), we are excited to announce that Pacific Blue Cross now offers electronic pre-determination and claims functionality for hearing products and services for MSDPR clients.
