Pre-determination is the new term for what was formerly referred to as a reserve.
Pre-authorizations are for specific services that require written pre-approval from Pacific Blue Cross prior to the provision of the services.
For the purposes of this FAQ, the term “pre-determination” will encompass both pre-determinations and pre-authorizations.
For eligible supplements, refer to the MSDPR Optician Supplemental Fees Schedule and the MSDPR Optometrist/Ophthalmologist Supplemental Fees Schedule.
Provider Registration/PROVIDERnet
-
How do I sign up for PROVIDERnet?
Detailed instructions on how to sign up for PROVIDERnet are available in the Vision Provider Reference Guide.
-
I am an optometrist who works at a few different stores. How should I get ready for this change?
You should ensure that you have one account per store location. If you do not already have one account per store location, please apply today. For pre-determinations and claims to go through, each store you work at must have its own account.
-
I have an optical store and we have an optometrist on site, how should I get ready for this change?
If you do not already have an optometrist provider ID for your store in addition to your optical store provider ID, please apply for one now.
-
Am I able to submit all pre-determinations and claims on PROVIDERnet?
Most of your pre-determinations can be submitted on PROVIDERnet, but not all. Some, along with their corresponding claims, will need to be submitted manually, including repairs and anything in the Fee Schedules that is listed in the “Additional Optical Services” and “Ministry Pre-Authorization Fee Codes” tables.
-
How can I check a client’s eligibility?
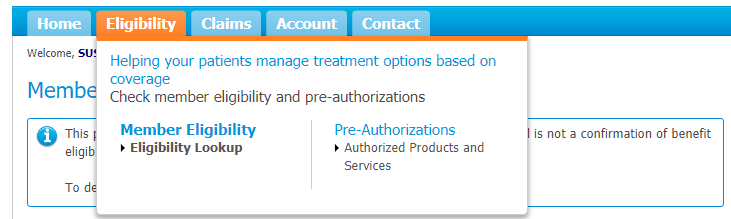
You can check a client’s eligibility by logging onto PROVIDERnet and clicking the Eligibility tab, then Member Eligibility. Select Eligibility Look up:
Please fill out the fields and click search:
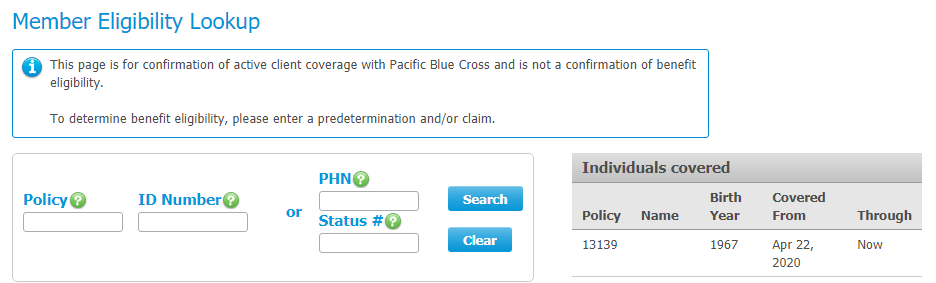
Please note: Coverage under the Ministry plan is determined on a month-to-month basis. Thus, you must always confirm the client is active for the current month when determining benefit eligibility. If you submitted a pre-determination in one month, but will submit the claim in the following month, please call to check eligibility prior to submitting the claim.
-
I have an optometrist’s clinic and we want to submit a pre-determination for a client on PROVIDERnet. Which practitioner should I select when I start the pre-determination?
Select the practitioner who helped the client.
-
Where can I find my provider number?
If you have previously submitted claims to Pacific Blue Cross, we have already assigned you with a provider ID. You can find this number in the top right-hand corner of your Claim Statement.
-
Do I need to use the same provider number on my pre-determination as well as my claim?
Yes. If you do not have the same provider number listed on both the pre-determination and claim, the claim will reject.
Pre-Determination/Claim Processing Information – For MSDPR client claims after March 11, 2021
-
What amount should I submit for my pre-determination/claim?
You must bill the actual product or service provided and the total amount (minus any client discounts).
-
How do I submit a manual pre-determination?
Use the new Vision form and check the pre-determination box. You can either fax or mail this form to us.
-
Can I fax my manual pre-determinations?
Yes. Fax pre-determinations to 1-604-419-2701 or 1-877-419-2196. Please make sure to submit each pre-determination separately, as we can only process one client ID at a time.
-
What details do I need to include when I submit a manual pre-determination/claim?
When you’re submitting a pre-determination/claim for any items other than eye exams (i.e. repairs, frames, etc.) indicate the type of glasses it is for.
-
Can I enter multiple types of glasses on one claim on PROVIDERnet?
Only enter one type of glasses per claim on PROVIDERnet. This means readers and distance glasses must be entered as two separate claim submissions.
-
I work in an optical store where we have an optometrist staff member. How do I submit a claim for an eye exam?
If you are using PROVIDERnet, submit the claim under your store’s optometrist Provider ID. You will also have to choose which optometrist provided the service.
If you are submitting the claim by paper, submit separately under your store’s optometrist Provider ID and include the name and Practitioner ID of the optometrist that provided the service.
-
I work at an optometrist’s office and want to submit an eye exam. How do I do this?
If you are submitting by PROVIDERnet, select the practitioner that performed the eye exam when you start the claim.
If you are submitting this claim by paper, indicate the practitioner that performed the eye exam.
-
How do I submit a pre-determination/claim for a balance lens on PROVIDERnet?
To submit this on PROVIDERnet, please twin the prescription from the other lens.
-
How do I submit a pre-determination/claim for plano lenses?
Please submit these pre-determinations/claims manually
Transition Information
-
What is changing?
We are offering electronic pre-determination and claims processing for vision products and services for MSDPR clients. This functionality is going live on March 12, 2021.
-
Why are you making these changes?
Through automation we can provide you with better service and help to streamline your administration of MSDPR clients by reducing your claims handling costs and turning pre-determination confirmations and benefit claims around faster.
-
I’m a vision provider. How will these changes affect me?
If you are registered for PROVIDERnet and direct deposit with Pacific Blue Cross, you will have the ability to process most product or service pre-determinations, as well as submit most benefits claims electronically on behalf of MSDPR clients. Plus, the direct deposit set-up ensures reimbursements from all Pacific Blue Cross plans are paid right into the bank account you set up on PROVIDERnet.
If you are not registered for PROVIDERnet, we encourage you to sign up to streamline pre-determinations and claims processing.
Reserve Information
-
Will reserves continue to be done for vision care benefits?
As of the launch date, the process formerly known as “reserves” will be called “pre-determinations” when submitting online and paper claims.
We will no longer be processing reserves for MSDPR clients by phone. We’ll be retiring the telephone reserve process and replacing it with the online and paper pre-determination process.
-
Will I be able to call the Client Service Centre to request a pre-determination after this new functionality is operational?
No. There will be two options to obtain a pre-determination for a vision care benefit: submit it electronically using PROVIDERnet or mail/fax us a paper-based pre-determination form.
-
What happens if I have submitted a reserve request prior to the launch of the new electronic processes in PROVIDERnet?
Vision reserves submitted prior to March 12, 2021 will be honoured up to 30 days after the launch date. You must submit claims for these reserves manually using the updated Vision form available on www.providernet.ca. We encourage you to submit a pre-determination to replace any reserves you already have on file to ensure that the client’s services will be covered and that you can submit claims on their behalf.
NOTE: All vision reserves by phone will expire by April 12, 2021, after which you’ll be required to submit a new pre-determination via PROVIDERnet or mail/fax.
-
Are pre-determinations required for an MSDPR client’s claim to be processed?
Yes. To secure eligibility and payment, all claims for vision products and services submitted on behalf of MSDPR clients must have an approved pre-determination on file to be processed for a claim and reimbursement.
-
Can I still fax you the completed pre-determination forms?
Yes. However, pre-determination outcomes will be mailed to you. If you have registered for PROVIDERnet, you’ll also be able to view the outcomes online.
General Inquiries
-
Which vision products and services are covered for MSDPR clients?
Pacific Blue Cross will continue to follow the MSDPR Optician Supplemental Fees Schedule and the MSDPR Optometrist/Ophthalmologist Supplemental Fees Schedule. Please review these documents to understand the coverage levels.
Some codes in the fee schedules will change to better identify services; some codes now are labeled “both,” while others are specific to right and left eyes. Please be sure to use the applicable code when you are submitting your pre-determination/claim.
-
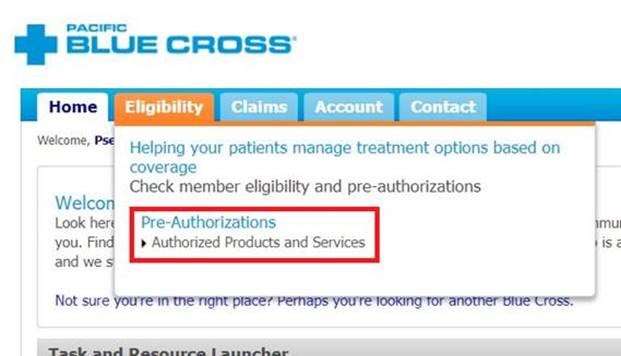
If you have PROVIDERnet, go to the Eligibility -> Authorized Products and Services:
Then find the pre-determination you wish to reverse by searching for the client. Once you’ve found the right pre-determination, click on Details:

You will see a button that allows you to reverse the pre-determination.
If you do not have PROVIDERnet, you have two options to reverse a pre-determination:
- Send a new, completed pre-determination form with all information matching from the original (e.g., the same provider and client information as well as the same services requested) that clearly indicates the request for a reversal.
- Send a copy of the pre-determination Explanation of Benefits (EOB) and add a note asking to reverse it.
-
How long do I have to reverse a pre-determination?
You can reverse pre-determinations up to the claiming deadline (one year from the date of service).
-
Can I reverse a pre-determination that is currently pended?
You are not able to reverse a pre-determination that is currently pended.
-
How do I submit a claim if the MSDPR client has coverage through another plan?
If the client has other coverage, please submit this claim manually and include the EOB you have received from their other coverage.
If the client’s other coverage is administered by Pacific Blue Cross, please submit a completed Assignment of Payment form along with a completed Ministry Vision form.
-
How long do I have to reverse a claim?
You can reverse claims up to the claiming deadline (one year from the date of service).
-
How do I submit for services rendered outside of BC?
These are handled on an exceptional basis and require manual submission. Complete a pre-determination and submit this by mail or fax.
-
Can I submit sight tests and refraction tests?
Sight tests and refraction tests are not eligible. For eligible supplements, refer to the MSDPR Optician Supplemental Fees Schedule and the MSDPR Optometrist/Ophthalmologist Supplemental Fees Schedule
-
Where can I find the pre-determination/claim form?
You can find the pre-determination/claim form at https://www.pac.bluecross.ca/pdf-bin/ministry/0606.001_MinistryClaimForm_VISION.pdf.
Please note that effective June 1st, 2021 manual submissions for Vision will require the new updated pre-determination/claim form. Claims received on old forms will no longer be accepted after June 1st, 2021.
-
What date do I enter on the prescription?
Please use the date the exam was performed on
-
What should I do with the cheque when there is a payment error on a bulk statement (more than one client)?
Please cash the cheque and report the error to the call center. The adjustment will appear on the next payment.
Specific Claiming Situations
-
How do I enter multiple items in one pre-determination?
Once you have entered the information for the first item, rather than selecting “Submit,” choose “Add Another Expense.”
Please note that pre-determinations for vision products only support one prescription (e.g. readers and distance) at a time. If you would like to pre-determine multiple products that require different prescriptions, please start a new pre-determination and submit each separately.
-
How do I submit a pre-determination when add-ons are required?
Once you have entered the information for the complete set or lenses, choose “Add Another Expense” rather than selecting “Submit”. Now you can enter the add-on(s) you require. Repeat this process as many times as necessary until you have added all applicable add-ons.
For example, you must add the cylinder twice if the prescription in each eye has a cylinder component.
-
How do I submit a pre-determination for an item that has a lab cost or requires a wholesale invoice?
Submit this pre-determination manually by mail or fax.
-
How do I submit prism pre-determinations and claims?
In order to submit prism claims, you must have a Base. If there is more than one kind of Base per eye, please submit these pre-determinations and claims manually.
-
What do I do when I receive a message that there is already a pre-determination on file for this expense?
Check your Authorized Products and Services screen. If you do not have a pre-determination on file for this client, they may have received a pre-determination from another provider. Have them contact the other provider to reverse the pre-determination, then try submitting again.
-
How do I submit a pre-determination based on a prescription change?
If there has been a change in the client’s refractive status, you can submit a pre-determination using the updated prescription for both eyes, even if there is only change in one eye.
Please note that there have been new left/right codes added, so be sure to choose the applicable code.
If your pre-determination is rejected, please see the question below for further information
-
If, after reviewing the MSDPR Optician Supplemental Fees Schedule and the MSDPR Optometrist/Ophthalmologist Supplemental Fees Schedule you feel that this claim should be eligible due to a prescription change, send in a completed pre-determination form by mail or fax for manual review. Please include the pre-determination ID from the rejected submission.
-
When I try to add a new prescription for a client, all of the values are set to (+) 0.00. What if I have a nearsighted client?
You can delete the default values in the prescription fields and rewrite as necessary. Therefore, if you have a nearsighted client, please enter their (-) values in these fields.
Please note that cylinder should always be in (-) format. If the prescription is not already in this format, please transpose it before entering it on PROVIDERnet.
-
If I enter a client’s prescription incorrectly on PROVIDERnet for a pre-determination, what should I do?
If an error was made when entering a client’s prescription, manually submit (by mail or fax) a new, completed pre-determination form with the correct prescription and a note about what happened. Ensure all of the other information matches the original, i.e. the same provider and client information as well as the same services requested.
-
How do I enter the prescription if the patient is receiving single vision glasses, but their current prescription is bifocal?
Simply transpose the prescription and enter the readers or distance prescription that applies to the claim.
-
Are progressive lenses eligible?
Progressive lenses are not eligible, but they can be paid as bifocal or trifocal lenses.
-
How do I submit for a lost, stolen, or broken item?
Manually submit (by mail or fax) a completed Vision form for a pre-authorization, which must include a detailed description of what is lost, stolen, broken, or damaged. For example, if the left lens is scratched, please indicate where on the lens it is scratched.
-
What should I do if I entered a pre-determination but forgot to include some service codes?
Please reverse the pre-determination that is missing some of the service codes and resubmit it.
For assistance with reversing a pre-determination, please see How do I reverse a pre-determination.
-
Why has my claim rejected when I have an approved pre-determination on file for the client?
Please ensure that your pre-determination and claim contain the same service codes. If they do not match, your claim will reject.
