-
What is changing?
We’re pleased to advise that we’ll be rolling out electronic claim and pay direct functionality for emergency dental services for MSDPR clients.
-
Why are you making these changes?
Through automation we can provide better service, help to streamline your administration of MSDPR clients, reduce your claims handling costs, and turn claims around faster.
-
I’m a dental Provider: How will these changes affect me?
If you are registered for PROVIDERnet and direct deposit with Pacific Blue Cross, you will have the ability to submit MSDPR emergency dental claims electronically through EDI and then request an emergency reassessment on PROVIDERnet— in most cases there will be no need to mail a paper-based claim. Plus, the direct deposit set-up ensures reimbursements from all Pacific Blue Cross plans are paid right into the bank account you set up on PROVIDERnet.
-
When will these changes take place?
Changes will roll out February 18, 2020.
-
How will I find out if a client is covered by the MSDPR plan?
Dental Providers can use PROVIDERnet to determine eligibility by keying in the patient’s Personal Health Number (PHN) and at least one fee number.
-
Can I still send claims in manually?
Yes.
-
Will there be any changes to benefits coverage for MSDPR clients?
No. Benefit coverage amounts are not changing; fees will continue to be paid according to the MSDPR Fee Guides (currently available on the Ministry's website or on pac.bluecross.ca/provider
-
How do I prepare for this transition?
Register as a Provider with Pacific Blue Cross and sign up for PROVIDERnet and direct deposit (which is managed through PROVIDERnet). You will need access to PROVIDERnet in order to process claims electronically and direct deposit to receive payments.
-
How do I sign up for PROVIDERnet?
To sign up for PROVIDERnet, go to the Dental Account Management page and follow the prompts.
Detailed instructions on how to sign up for PROVIDERnet are available in the Dental Provider Reference Guide found on pac.bluecross.ca/provider.
-
How do I sign up for direct deposit or make changes to my existing information?
You must be registered with PROVIDERnet to set up or manage direct deposit. Detailed instructions are available in the Dental Provider Reference Guide at pac.bluecross.ca/provider.
-
Will I get paid as soon as the claim is adjudicated?
No. Payment dates will remain the same as other Pacific Blue Cross plans. However, instead of mailing a cheque we’ll deposit the reimbursement directly into the bank account you set up on PROVIDERnet.
-
How can I confirm MSDPR client eligibility for dental services?
MSDPR clients will have either a British Columbia Driver’s Licence or British Columbia Services Card as their identification.
This card will contain their Personal Health Number (PHN), which is unique to each individual. The policy number for MSDPR clients is 13139. To be eligible for coverage, MSDPR clients must reside in British Columbia.
-
Which dental services are covered for MSDPR clients?
Clients eligible for Ministry-sponsored dental coverage from Pacific Blue Cross will have one of the following coverage levels:
- Basic dental services with a two-year limit; as well as additional coverage for emergency services for the relief of pain once that limit has been exhausted
OR
- Emergency services coverage only, for the relief of pain (no basic dental services coverage)
To understand how the differences between coverage types can affect claiming procedures, please review the Pacific Blue Cross Dental Reference Guide.
-
How do I know which level of MSDPR coverage my patient has?
You have two options to assess your patient’s Ministry coverage:
- Determine eligibility in PROVIDERnet by keying in the patient’s Personal Health Number (PHN), as well as at least one fee number. Make sure to check for the policy number to determine Ministry Coverage (the policy number for MSDPR clients is 13139).

- Contact Pacific Blue Cross at 604-419-2000 (toll-free: 1-877-722-2583), Monday to Friday 8:00 am to 4:30 pm (excluding statutory holidays).
- Determine eligibility in PROVIDERnet by keying in the patient’s Personal Health Number (PHN), as well as at least one fee number. Make sure to check for the policy number to determine Ministry Coverage (the policy number for MSDPR clients is 13139).
-
How do I submit an emergency claim for an MSDPR client?
To submit an Emergency coverage claim to Pacific Blue Cross, you must first submit it through CDAnet®/DACnet™ as you would a regular ministry claim. This can be done even if the patient has emergency services only coverage (no basic services coverage). The claim will not pay initially. Note: If you receive a “pending” result from CDAnet®/DACnet™, you will need to wait for their adjudication before proceeding.
Once the claim has been processed (whether partially paid from existing basic services coverage, or not paid), it will appear in the client’s Claims History in PROVIDERnet.
After entering your initial claim request in CDAnet®/DACnet™, you should see the claim appear in the client’s Claims History in PROVIDERnet within minutes.
Emergency Claim Resubmission Walkthrough
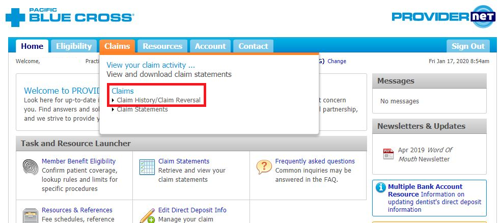
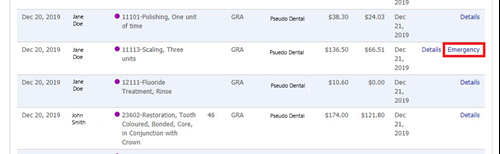
- After processing the claim in CDAnet®/DACnet™, log in to your PROVIDERnet account
- Click the Claims tab at the top, then choose Claim History/Claim Reversal.
- Locate the claim you wish to resubmit for Emergency Coverage, then click Emergency in the right-hand column.

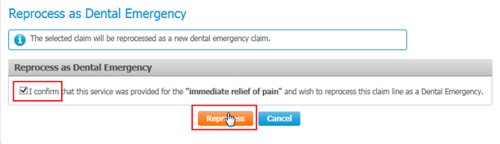
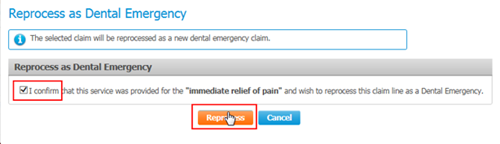
- Confirm that this service was provided for the “immediate relief of pain” by clicking the check box and then click on the Reprocess button
Your claim will now be reprocessed as an Emergency Coverage claim, and you will receive your payment and statement electronically.
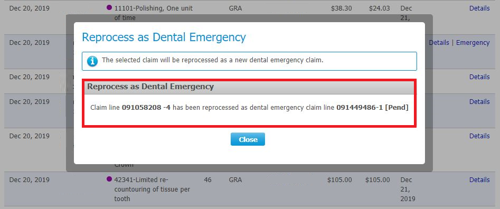
Note: Once the claim has been resubmitted, if you select “Emergency” again, you will receive confirmation that the claim has been reprocessed. No further action is required.
- After processing the claim in CDAnet®/DACnet™, log in to your PROVIDERnet account
-
Can all MSDPR Emergency Coverage claims be processed electronically?
Not all fee codes eligible for emergency services coverage (such as certain periodontal services) will be able to be resubmitted through PROVIDERnet. As outlined in the relevant Fee Schedules, Emergency Coverage Claims can still be submitted on a standard, computer generated or Pacific Blue Cross claim form.
FAQ: Ministry of Social Development and Poverty Reduction – Digital management of emergency dental claims
As the benefits administrator for the Ministry of Social Development and Poverty Reduction (MSDPR), we are excited to announce that Pacific Blue Cross will be rolling out electronic claim and pay direct functionality for emergency dental services for MSDPR clients on February 18, 2020.

Step-by-step guide to submitting an Emergency Claim for MSDPR clients
There are a few different steps you’ll need to take when submitting an Emergency Claim for an MSDPR client, including first submitting a claim through CDAnet®/DACnet™ (business as usual).
Emergency claims can be done even if the patient has emergency services only coverage (no basic services coverage). Please note:
- The claim will not pay initially. If you receive a “pending” result from CDAnet®/DACnet™, you will need to wait for their adjudication before proceeding.
- Once the claim has been processed (whether partially paid from existing basic services coverage, or not paid), it will appear in the client’s Claims History in PROVIDERnet.
- After entering your initial claim request in CDAnet®/DACnet™, you should see the claim appear in the client’s Claims History in PROVIDERnet within minutes.
Emergency Claim Resubmission Walkthrough
- After processing the claim in CDAnet®/DACnet™, log in to your PROVIDERnet account.
- Select the Claims tab from the top menu, then choose Claim History/Claim Reversal.

- Locate the claim you wish to resubmit for Emergency Coverage, then click Emergency in the right-hand column.
- Confirm that this service was provided for the “immediate relief of pain” by clicking the check box and then click on the Reprocess button.
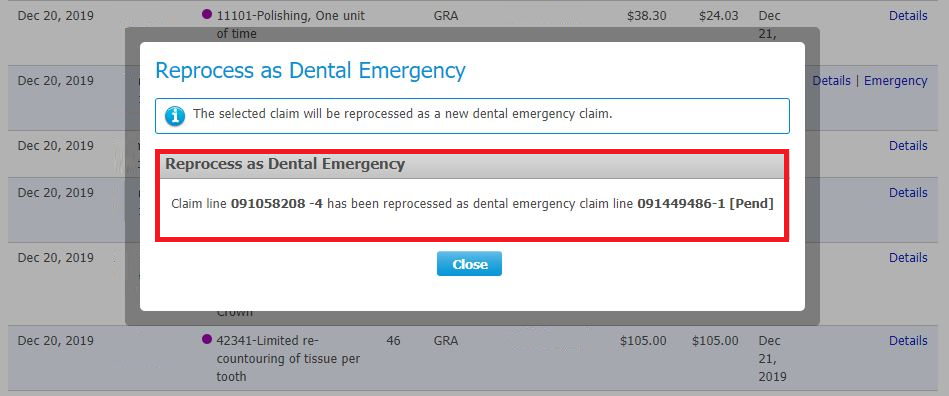
Your claim will now be reprocessed as an Emergency Coverage claim, and you will receive your payment and statement electronically.
Note: Once the claim has been resubmitted, if you select “Emergency” again, you will receive confirmation that the claim has been reprocessed. No further action is required.