Prior Authorization for High Cost Drugs
Sunday, Mar 26, 2017Certain drugs require prior authorization to confirm intended use and to ensure full or partial reimbursement...
High cost specialty drugs are used by a small number of members but the cost to health plans is significant and growing. To help manage these costs, and to ensure the sustainability of your health plans, we implemented a Prior Authorization Program for High Cost Drugs.
This means, for drugs included in the Prior Authorization Program for High Cost Drugs, we will require prior authorization forms to be submitted and approved before we can reimburse prescriptions costs.
What are the benefits of this program?
- Helps prevent increases in insurance premiums by protecting your benefit plan from escalating drug costs
- Ensures these drugs are taken appropriately at the right place in therapy and have been prescribed according to Health Canada recommendations.
- May save you some out-of-pocket costs for expensive drugs.
How do I submit a prior authorization application?
- You will likely be notified by your pharmacist or a drug manufacturer’s Patient Assistance Program that your medication requires prior authorization.
- Download the corresponding prior authorization form for your type of drug. The form needs to be completed by your physician.
- Fax the completed form to the fax number indicated at the top of the relevant form.
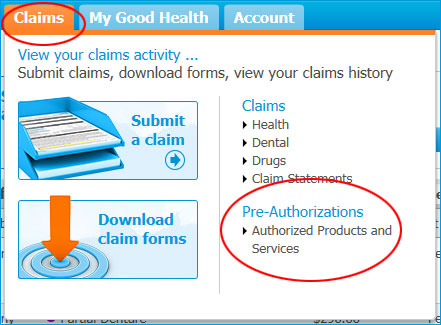
- For drugs that require PBC Prior Approval: We will review the form and make a decision within 5 business days in most cases. You will then be informed of our decision. You can also view approvals in your Member Profile in Claims » Pre-Authorizations
For drugs that require BC PharmaCare Special Authority Approval: If approved by BC PharmaCare, no further action is required. PBC will receive notification of the approval electronically at the time the claim is processed by the pharmacy.
The drug manufacturer’s Patient Assistance Program and pharmacies in our Preferred Pharmacy Network can assist you with this process.
High Cost Drugs Requiring BC PharmaCare Application
BC PharmaCare provides prescription drug coverage for all British Columbians through its Fair PharmaCare program. Each drug undergoes a thorough medical and patient review process before it is added to the list of covered drugs. By aligning with BC PharmaCare coverage, we can ensure that your group drug plan is being managed as sustainably as possible.
Certain drugs require that your doctor apply to BC PharmaCare Special Authority before they are eligible with your plan. If you have a prescription for one or more of these high cost drugs, it will require an application to BC PharmaCare before it will be considered under your drug plan. Once you have been approved, you will not have to send paperwork to Blue Cross – instead, you can use your pay direct drug card for instant claiming at BC pharmacies. If your request for a BC PharmaCare Special Authority is denied, please send a copy of the denial to us for further review.
Prior Authorization Forms for High Cost Drugs
These forms need to be completed by your physician.
If your drug has not been approved
If coverage for your prescription has not been approved through the BC PharmaCare Special Authority Program or another Government Agency, then please submit the decision along with the completed Drug Eligibility Inquiry Form below. Drug coverage can vary between Extended Health Plans. We will review the information provided for eligibility under the provisions of your specific Extended Health Care plan.

 .
.